B.C. turns down Alberta's call for COVID-19 help amid serious hospital crunch
A day after one of Alberta’s top health officials announced that that province’s COVID-19 health-care crisis necessitated a cross-country call for help, British Columbia’s health minister has responded to say B.C. simply can’t handle helping anyone else.
On Wednesday, Alberta declared a public health emergency and Premier Jason Kenney apologized for ignoring the warnings of experts and lifting nearly all public health measures over the summer, a decision that led to a surge in COVID-19 cases now that threatens to overwhelm staffed intensive care beds within 10 days.
“We are taking two extremely difficult steps: We will be reaching out to other provinces to see if they have any available ICU space where Albertans could get the care that they need, as well as asking them if they have skilled frontline staff who may be willing to come to Alberta to assist us,” said Alberta Health Services president and CEO Dr. Verna Yiu at the news conference where the public health emergency was declared.
“We remain hopeful that it will not come to this, as we continue to add critical care capacity.”
On Thursday, CTV News Vancouver asked the ministry of health whether B.C. would be able to help its neighbouring province, but the answer was “no.”
“Given the current demands on B.C.’s health-care system, we will not be able to assist with taking patients at this time,” said B.C. Minister of Health Adrian Dix in an email statement.
“If we can take patients on in the future, we will.”
Ontario, which has far fewer active COVID-19 cases than all of Western Canada on a per-capita basis, has offered to assist Alberta.
ICUS IN B.C. STRUGGLING TO HANDLE LOCAL PATIENTS
Frontline health-care workers who spoke with CTV News aren’t surprised the province had to turn down the request for assistance, painting a picture of intensive care units that are struggling to handle the influx of local COVID-19 patients.
In Northern Health, in particular, the situation is so dire that one doctor described the system as “close to collapse.”
Rather than one-on-one care for critically ill patients, nurses are now working in teams with multiple patients for each nurse; there are concerns patients are not receiving the level of care they require, and the stress on those who work is said to be contributing to nurses avoiding or refusing ICU shifts.
Some nurses have left the profession altogether. Others have stepped away from full-time work to take on-call shifts where they aren’t pressured to work as much overtime and can take on as much work as they want.
Doctors and nurses alike describe the growing staff shortages and protests in front of hospitals as fraying nerves further, at a time more COVID-19 patients – the vast majority of them unvaccinated – are needing medical care.
All who spoke to CTV News expressed deep regret and frustration that so many people needing medical care for health issues unrelated to the pandemic are having to wait, sometimes to deadly effect.
ONTARIO NOW OUTPERFORMING WESTERN CANADA WITH CAUTIOUS APPROACH
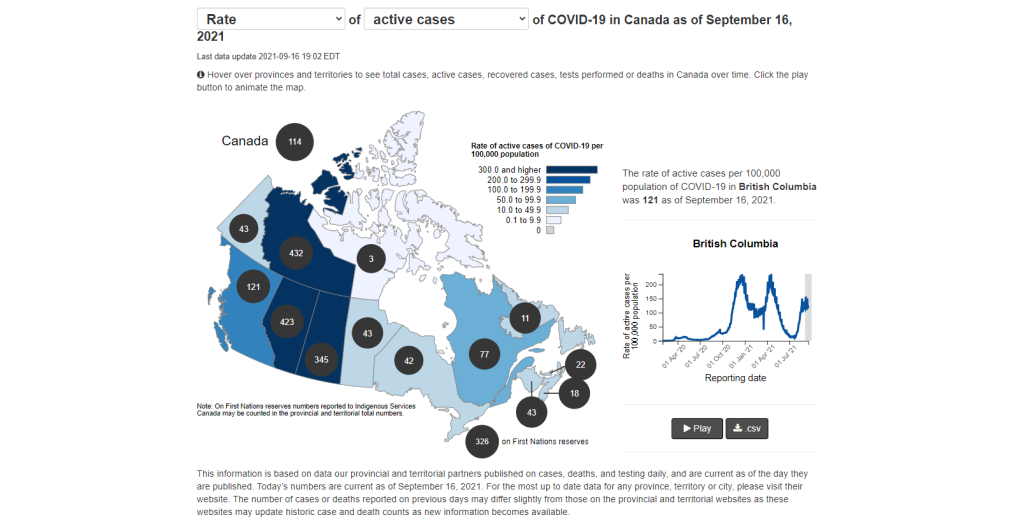
The Public Health Agency of Canada COVID-19 dashboard illustrates in stark contrast how provinces’ different pandemic management approaches and philosophies are playing out.
In Ontario, where there are more safety measures for schools and a mask mandate for indoor public spaces remained in place through the summer, there are currently 42 active cases per 100,000 people. There are 121 in British Columbia and 423 in Alberta, with 345 per 100,000 in Saskatchewan.
Alberta’s top doctor hinted that the poor performance of western provinces compared to Ontario may not be coincidence, describing discussions between the provinces as they all lifted public health measures (to varying degrees) at the start of the summer.
“The three western provinces all moved to release restrictions,” said Dr. Deena Hinshaw, Alberta’s chief medical officer of health, adding her decision was based, in part, on discussions with colleagues.
“All of us were looking at the data, and all of us believed that we would see a decoupling, similar to what was seen in the U.K. “
While the proportion of confirmed infections compared to hospitalizations is lower than in previous waves, the fourth wave has still seen an influx of COVID-19 patients to hospital needing oxygen support and, sometimes, ventilated machine breathing.
And, while health officials are now keen to point out the majority of infections are in unvaccinated people, in order to encourage everyone to get the protection resulting from full vaccination, B.C. experts had warned months ago that lifting restrictions too early amid the ultra-contagious Delta variant could see a pandemic fuelled by those who had no protection and were much more likely to end up in hospital.
CTVNews.ca Top Stories

LIVE UPDATES Taylor Swift hits the stage at Rogers Centre for first night of Eras Tour in Toronto
Taylor Swift takes the stage at the Rogers Centre as 'The Eras Tour' has arrived.
Purolator workers won't handle Canada Post packages if strike occurs, union says
Teamsters Canada says if Canada Post workers go on strike or are locked out, its members at Purolator won't handle any packages postmarked or identified as originating from the carrier.
Trump chooses anti-vaccine activist Robert F. Kennedy Jr. as health secretary
U.S. President-elect Donald Trump says he will nominate anti-vaccine activist Robert F. Kennedy Jr. to lead the Department of Health and Human Services, putting him in charge of a massive agency that oversees everything from drug, vaccine and food safety to medical research and the social safety net programs Medicare and Medicaid.
Canada urged to cut government-funded research collaborations with China: report
A newly released report is urging Canada to immediately end all government-funded research collaborations with China in a variety of different areas.
Centre Block renovation facing timeline and budget 'pressures'
The multi-billion-dollar renovation of parliament’s Centre Block building continues to be on time and on budget, but construction crews are facing 'pressures' when it comes to the deadline and total costs, according to the department in charge of the project.
Winnipeg driver rescues passengers from burning van
A Winnipeg driver was in the right place at the right time when a paratransit van caught fire Thursday morning.
B.C.'s chief vet tells clinics to set up bird flu protocols amid human exposure risk
British Columbia's chief veterinarian has told clinics that treat wild birds that they must establish protocols to prevent the spread of avian flu, warning of the risk of human exposure to the illness.
Measles cases in New Brunswick continue to climb
The number of measles cases in New Brunswick continue to climb. Officials with New Brunswick’s Department of Health said as of Thursday, the number of confirmed cases since October has reached 43.
Police release bodycam video of officer-involved incident at Hindu temple protest in Brampton, Ont.
Police say an officer who forcefully removed a 'weapon' from a protester outside of a Hindu temple in Brampton was acting 'within the lawful execution of his duties' after bystander video of the incident circulated widely online.