About two years ago, seemingly out of the blue, Susan Drury was struck with severe osteoarthritis in her right hip.
The 57-year-old West Vancouver resident started working with a physiotherapist, but as time went on her aches only got worse. Osteoarthritis was developing in Drury’s left hip as well, and she eventually had to rely on a cane to get around.
“It was extremely painful,” she said. “I had a permanent limp. I couldn’t bear any weight on my right leg when I stood up.”
After learning about the long waitlist for treatment at home – from seven to nine months – Drury decided to join a growing number of Canadians who are turning to the pricey practice of medical tourism.
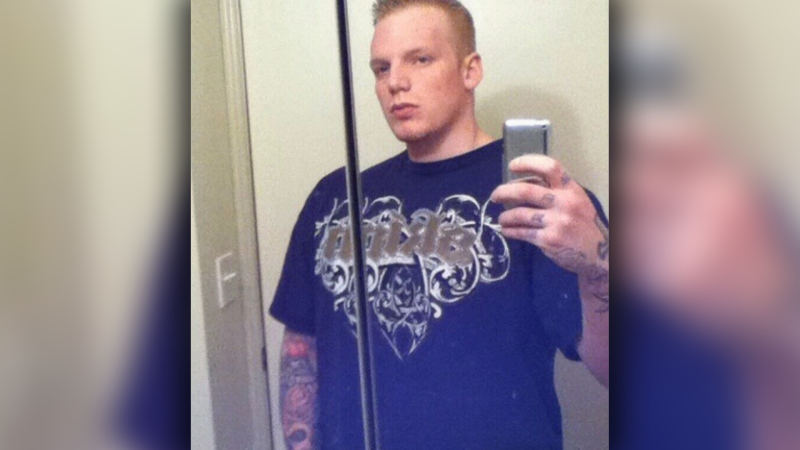
Drury first got in touch with Timely Medical Alternatives, a private Vancouver business that specializes in connecting Canadian patients with U.S. hospitals.
Founder Rick Baker said he’s helped about 2,000 people find treatment south of the border, mainly for hip replacements, knee replacements, spinal surgeries or gynecological procedures.
Though frustrating wait times drive a lot of his clientele, Baker said they’re not the only factor.
“You have a choice of the technique, you have a choice of the time when it’s done, you have a choice of surgeons,” he said. “We have access to 22 orthopedic surgeons in the U.S., and all of them have CVs so you can read about their training, their experience”
Prices vary depending where you go. Timely Medical Alternatives deals only with American facilities, though there are similar services that look further abroad to destinations such as India, Thailand and Cuba. Some patients also opt to research international treatments on their own.
Baker said hip and knee replacements run about $65,000 apiece in the U.S., but through his relationships with health care providers he can secure them for $22,000 – a price that would still look steep to many who are accustomed to universal health care.
The practice of travelling outside Canada for medical treatment isn’t generally illegal. Unfortunately, researchers say the practice isn’t tracked, traced or regulated either.
“When you fill out your customs form, you’re never asked if you went abroad for medical care,” said Dr. Valorie Crooks, an associate professor at Simon Fraser University.
“We actually don’t have a mechanism to trace these individuals.”
Crooks, who has been studying medical tourism with a team at SFU since 2009, said there are pitfalls to the lack of oversight. For one thing, the majority of medical tourism patients require additional care back home, even follow-up surgery or rehab, which can catch local health care providers by surprise.
“When we don’t know how many people are going abroad, then it becomes difficult for us to anticipate those needs,” Crooks said.
Canadian doctors have also complained that they have no idea what their responsibilities are when a patient asks for advice about travelling for treatment, or what legal issues are involved.
Crooks said policy makers are reluctant to discuss medical tourism, however, because of concerns they’ll be perceived as supporting or encouraging it.
“This is why these provincial and national conversations are not happening, and why our individual physicians are left on a case-by-case basis to determine if and how they will engage in a dialogue with their patients about medical tourism,” she said.
Drury was eventually sent to South Dakota, where she was able to get both hips replaced at once for about $36,000.
For her part, despite the high cost, the results were well worth it.
“I have no regrets, that’s for sure,” Drury said.
With a report from CTV Vancouver’s Maria Weisgarber