VANCOUVER -- Frontline medical workers, administrators and others are painting a troubling picture of the state of B.C. hospitals, with some intensive care units full and contingency plans underway as staff struggle to keep up with incoming COVID-19 patients.
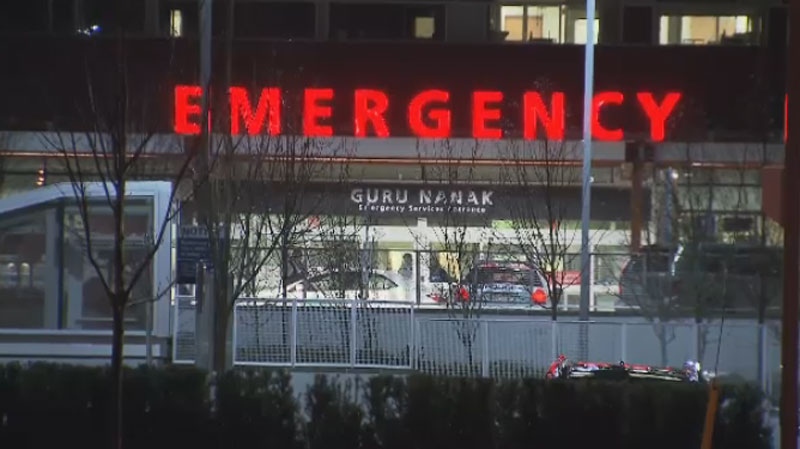
In Fraser Health alone, there are 229 COVID-19 patients, with 67 of them in ICU and high acuity units. Approximately half of them are at Surrey Memorial Hospital, and the health authority is operating at 96 per cent hospital capacity overall, with some hospitals at 100 per cent.
Five of the 60 operating rooms normally run by Fraser Health have been already closed so that staff could be diverted to COVID-19 care, according to Dr. Victoria Lee, president and CEO of the health authority. That's forced dozens of non-emergency surgeries to be postponed.
“What that might look like would be 50 to 70 actual surgeries," Lee said Tuesday. "I think we talked about how painstaking some of these decisions are."
B.C.'s health minister described the situation in clinical terms on Monday, which didn’t express the reality inside hospitals, according to several frontline workers who spoke to CTV News publicly and on background.
“We are looking at a number of hospitals around B.C. and moving into the utilization of surge beds, requiring a degree of service deferral to support staff redeployment to support our existing staff and to deal with the pressures of COVID-19 admissions,” said Adrian Dix.
But the president of the BC Nurses’ Union said she polled her members Monday morning and those working at the major hospitals in the province said their base beds are all full.
“In many cases they were over full,” said Christin Sorensen. “This is what the minister describes as surge capacity — they are people who are placed in hallways, in waiting rooms, in shower rooms, sunrooms, they spend extended periods in an emergency room because they cannot be moved to an in-patient unit on the floor.”
Less critical or non-COVID patients are being transferred to less busy hospitals as key facilities fill up. The Ministry of Health’s presentation on Monday showed Abbotsford Regional Hospital, Surrey Memorial, and Vancouver General hospitals have less than five per cent capacity in medical and ICU units; only 23 base beds are empty in the Lower Mainland, according to that information.
Despite these statistics and issues, the emergency field hospital set up at the Vancouver Convention Centre still hasn’t been used; it had been set up last spring and earmarked for non-COVID patients to be sent there on a referral basis.
“It is ready to be operationalized, and can begin accepting patients within 72 hours, should the need arise,” wrote a spokesperson.
Monday’s ministry presentation pointed out they’d forecast four pandemic scenarios for the fall and winter, with the worst-case scenario: “High++ COVID-19 case (the number of COVID-19 new cases and admissions mirrors a more extreme scenario with twice as many cases as during the March-May epidemic experience) – ICU 214/Acute 400 occupancy.”
On Tuesday, the province's COVID-19 hospitalizations reached a new record high of 456, with a record 148 patients in ICU.
Challenges put in writing
A doctor from Royal Columbian Hospital wrote a public Facebook post over the weekend, describing assessing a sick patient on the floor.
“She was in the Covid area and after waiting four hours was feeling so faint she decided it was better to lay on a disgusting emergency floor than to collapse,” wrote Dr. Kelly Kasteel in the post. ”Covid patients who are transferred in by ambulance because their oxygen is critically low are waiting 3 hours for a bed. ICU's are refusing our transfers out because they literally have no space to care for patients. This is dangerous care. Nothing about this situation is acceptable.”
There are also correspondences that let stakeholders and staff know, in stark terms, just how precarious the situation is.
“Presently the Critical Care Capacity is very slim, as such electric cardiac procedures may nee do be deferred at any time to enable us to continue to provide that service,” reads an internal memo to Providence Health Care staff titled “COVID Third Wave Surge.”
In an email to donors of the Victoria Hospitals Foundation on Friday with the subject line “Our ICUs Are at Full Capacity, Can You Help?”, the executive director laid out a grim situation.
“Our ICUs are full and embarking contingency plans,” wrote Avery Brohman, who cited comments by the VP of clinical operations for Island Health, Elin Bjarnason.
“The only reason we are doing OK is the new temporary High Acuity Unit we have in place,” Bjarnason said of the unit at Royal Jubilee Hospital.
Caring for patients in a COVID ward is much more time-consuming, logistically challenging and dangerous than other patients for health-care workers, even though most of them are now vaccinated. The same precautions they were using six months ago, including layers of personal protective equipment and the use of binoculars, remain in place now.
Doctors and nurses at the point of exhaustion
Despite these challenges, the president of the Doctors of BC is urging anyone who needs medical help to seek it out.
“It’s important for the public to understand we still have capacity to deal with emergencies and with people’s medical needs,” said Dr. Matthew Chow. “We do not want people to be deferring important medical needs, if they’re having symptoms, if they’re having an emergency for sure make use of the health-care system.”
But he acknowledged the fatigue and strain many doctors are now under.
“Health-care workers — we’re human, we get tired, we need sleep, we need time to recharge, we need time with our families,” he pointed out. “Everything people can do to keep themselves safe — whether it’s trying not to injure themselves during their home improvement project with power tools they haven’t used in a while, or more importantly taking really good care to stop the spread of COVID right now — it’s supremely important.”
Sorensen echoed those comments, pointing out while there are ventilators and other equipment available, there’s been no significant increase in the qualified staff able to operate them and care for sick patients. Nurses are already working many overtime shifts, which is unsustainable, and prompted an urgent plea.
“If the public health guidelines are not followed, our healthcare system could be even more stretched than we are right now and we could be facing a situation similar to Ontario, where difficult decisions are having to be made about patient care, whether it happens or it’s denied,” she said. “We are at a breaking point, we’re in a difficult situation and we’re teetering on slipping into an area that could be disastrous for British Columbia unless we all do our part.”