B.C.'s COVID long haulers: Some paying for treatment, all looking for answers
Some British Columbians who were among the first to become infected with a mysterious global virus that didn’t yet have a name are marking two years of lingering symptoms.
In March 2020, the idea that COVID-19 symptoms could last long after the acute, infectious phase of the illness was approached with skepticism by many medical professionals. Now, researchers and clinicians have learned much about the virus and what it can do to the human body.
“Long COVID syndrome is more and more clearly (involving) almost every system in the body, including the nervous system,” said Dr. Chris Carlsten, UBC’s head of respiratory medicine and one of the first doctors to treat patients with ongoing symptoms.
“This not in their head. This is not something that they're making up and scientists and biologists and those that are spending time doing this are seeing real effects in the body that can explain it, even if we haven't come up with a treatment yet."
Carlsten says researchers now believe that the inflammation and damage different parts of the body could be due to the virus continuing to be active in those patients, that the immune system’s response plays a role, or that the antibodies generated could be responsible.
He emphasized that the approved COVID-19 vaccines are dramatically reducing the likelihood of developing long COVID, even if someone is infected, and that long-haulers who are vaccinated often see an improvement in their symptoms; time and targeted treatment are also helping.
“On average, the patients that come through the (provincially-funded COVID-19) clinics do seem improved and while we will analyze that statistically, formally, I am confident that we're seeing that," said Carlsten.
THE STRUGGLE TO BE BELIEVED
With symptoms ranging from physical (a never-ending cough or shortness of breath to muscle weakness) to neurological and mood-oriented (inability to concentrate, depression, PTSD), patients have struggled to get help from family doctors and walk-in clinics.
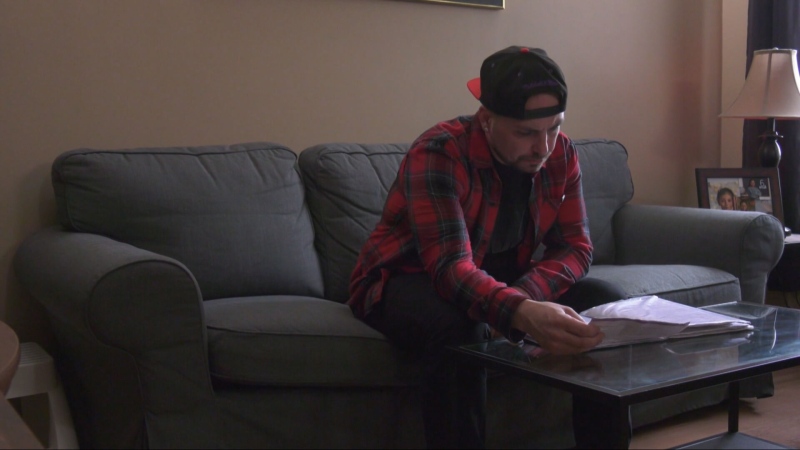
“I had to fight to be believed and it was a process that lasted at least a year," said Burnaby resident Jonah McGarva.
He got sick in March 2020 and was later diagnosed with early-onset emphysema, ultimately gaining access to one of the few dedicated long COVID clinics in the province.
“I was healthy, freshly married, planning to start a family, and literally within two weeks, three weeks, it was robbed from me,” he said. “I couldn't get out of bed. (I had) many nights when I didn't know if I would wake up the next day."
He co-founded an advocacy group, Long COVID Canada, and is pleading with the province to open more clinics to support long-haulers, whether their symptoms are debilitating and keep them from working and living a normal life, as in his case, or milder and allowing them to muddle along.
"This is a problem that we as a country are going to have to face at some time or another: that long COVID is a mass disabling event, worldwide," said McGarva, noting that some members in the support group have spent up to $20,000 seeking alleviation of their symptoms.
PRIVATE CLINICS FILLING THE VOID
Psychologists and physiotherapists are typically not covered by the public health-care system, but there are now other for-profit companies and care providers offering potential therapies for struggling long-haulers.
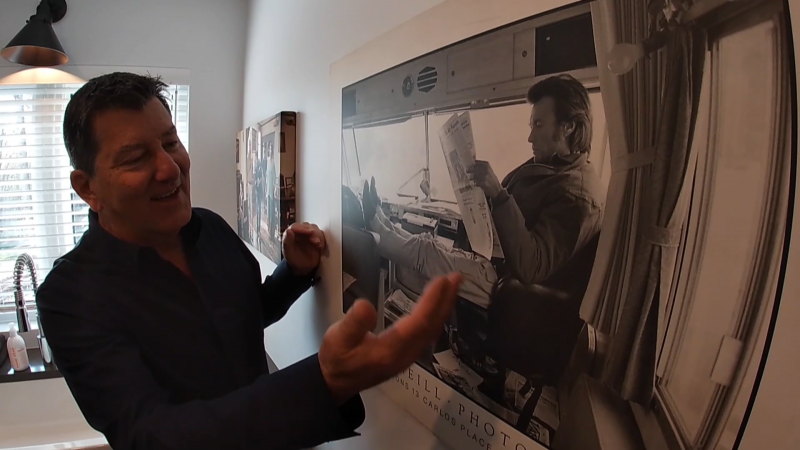
Langley-based ABI Wellness is a private clinic that’s been providing brain-injury recovery programs for years, but has recently begun offering its programs to long COVID sufferers.
"What the research shows is it presents similarly to brain injury, and what this brain fog that everyone keeps referencing, the conversation really should be moving to it being a COVID brain injury," said Shaun Porter, ABI’s chief operating officer.
While he wouldn’t detail how much a patient might pay for the computer-based cognitive exercises or how effective they’ve been so far, he said the virtual group discussion sessions have been therapeutic.
"A lot of individuals with long COVID are feeling gaslighted or not represented or heard properly by the medical field, so a key first step is letting them know this is a safe space,” said Porter. “They're being heard, they're being understood."
Last year, the province expanded its government-funded clinic system with teams of specialists, but the health minister told CTV News he wants the health-care system to support patients of all stripes and needs rather than focus solely on more dedicated long COVID clinics.
"I would expect, yes, that you'll see that," said Adrian Dix of the expansion of long COVID clinics.
“But you'll never be able to open up enough clinics to address all of that problem. You need the system to respond – to see it and to take advantage of the best possible research."
CTVNews.ca Top Stories

Poilievre will do 'anything to win,' must condemn Alex Jones endorsement: Trudeau
Prime Minister Justin Trudeau is ramping up his attacks on Conservative Leader Pierre Poilievre as he promotes his government's federal budget.
'My stomach dropped': Winnipeg man speaks out after being criminally harassed following single online date
A Winnipeg man said a single date gone wrong led to years of criminal harassment, false arrests, stress and depression.
New evidence challenges the Pentagon's account of a horrific attack as the U.S. withdrew from Afghanistan: CNN exclusive
New video evidence uncovered by CNN significantly undermines two Pentagon investigations into an ISIS-K suicide attack outside Kabul airport, during the American withdrawal from Afghanistan in 2021.
'One of the single most terrifying things ever': Ontario couple among passengers on sinking tour boat in Dominican Republic
A Toronto couple are speaking out about their 'extremely dangerous' experience on board a sinking tour boat in the Dominican Republic last week.
All Alberta wildfires to date in 2024 believed to be human-caused: province
There are 63 wildfires burning in Alberta's forest protection area as of Wednesday morning and seven mutual aid fires, including one in the Municipal District of Peace.
7 surveillance videos linked to extortions of South Asian home builders in Edmonton released
The Edmonton Police Service has released a number of surveillance videos related to a series of extortion cases in the city now dubbed 'Project Gaslight.'
Suspects waving weapons, smashing glass in Toronto jewelry store robbery caught on video
Arrests have been made after five men were captured on video rampaging through a jewelry store in Toronto, waving weapons and smashing glass display cases.
Pilot proposes to flight attendant girlfriend in front of passengers
A Polish pilot proposed to his flight attendant girlfriend during a flight from Warsaw to Krakow, and she said yes.
Ottawa injects another $36M into fund for those seriously injured or killed by vaccines
The federal government has added $36.4 million to a program designed to support people who have been seriously injured or killed by vaccines since the end of 2020.