100 open heart surgeries postponed in B.C. as critical COVID-19 patients vie for 'last resort' machines
Some 100 British Columbians have had their open-heart surgeries postponed in the past two months due to a shortage of critical resources required by the sickest COVID-19 patients, according to sources within the medical system.
When CTV News Vancouver asked the Provincial Health Services Authority about the estimate, the authority did not deny its accuracy, but insisted that the most dire cardiac procedures are still taking place at the same rate as usual.
“From February 2020 to May 2021, no critical cardiac surgeries were postponed in B.C.,” wrote a spokesperson in an email. “With the focus on urgent and critical cases, B.C. was able to ensure that all cardiac surgical procedures were completed aligned with recommended wait time targets.”
But the agency that oversees such procedures, Cardiac Services BC, also acknowledged that Lower Mainland cardiac care has been affected during the pandemic, though it declined to provide statistics.
The agency did not respond when asked how many people were currently on waiting lists, how many hospitals have been unable to treat urgent cardiac patients and redirected them to other hospitals, and how many people had died while waiting for serious cardiac procedures.
While many surgeries have been cancelled due to hospitals being nearly overwhelmed by COVID-19 patients during the third wave, sources tell CTV News open heart surgeries have been disproportionately affected and will be much harder to recover from due to a critical shortage of equipment and specialized staff described by doctors as a “last resort.”
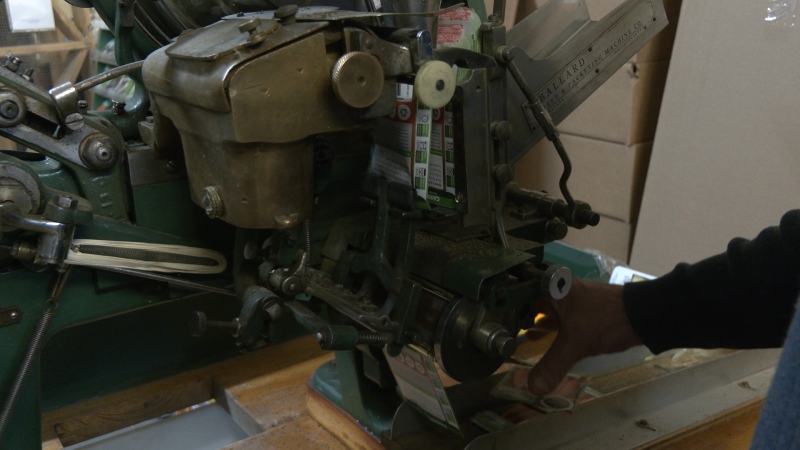
When COVID-19 patients aren’t responding to mechanical ventilation machines that breathe for them, they are sometimes placed on an Extra Corporeal Membrane Oxygenation (ECMO) machine, which removes the blood from the body and infuses it with oxygen before sending it back inside the body. A team of doctors and specialist technicians, called pulmonary perfusionists, are required to run the machine and keep the critically ill patient alive.
ECMO machines and perfusionists are also necessary during open heart surgeries, but with coronavirus patients needing them more urgently, scheduled surgeries have dropped dramatically, so that only the sickest cardiac patients are still getting their surgeries.
“Our critical care team in B.C. has been coordinated from the very beginning of this pandemic and has been working with both the cardiac and with the COVID response, the ICUS, to make sure they're available for people who need them,” said provincial health officer Dr. Bonnie Henry when CTV News asked what the plan was for cardiac patients.
She also said she was unaware of whether anyone had come to harm as a result.
In Manitoba, health officials confirmed five patients on the cardiac wait list died in recent months, and such patients are now being airlifted to hospitals outside the province for urgent medical care. In Ontario, doctors faced unprecedented demand for ECMO from COVID-19 patients and a public policy think tank says people have died as a result.
A RARE BUT IMPORTANT MACHINE IN SHORT SUPPLY
ECMO machines are in short supply. They’re usually used for organ transplants, on deathly ill patients and during open-heart surgeries, so Roland Clifford found himself on one five years ago when he went to hospital and was told he needed emergency cardiac surgery.
“They told me I had a widowmaker,” the senior recalled. “I spent eight days in hospital.”
Clifford said he was pushed down the list by other, more critical patients, but also bumped someone who was there before him.
"I didn't know that I had a problem,” he said. “It's different if you know you've got a problem and you know there's a fix and you've got to wait."
Clifford now volunteers with the Pacific Open Heart Association, which provides support and companionship to incoming cardiac patients. He has tremendous empathy for those waiting anxiously for the call for the life-changing, life-saving surgery.
"It's like taking an old car in and getting a complete overhaul of an engine,” he said. “Everything is great afterwards and they've got that to look forward to, which other patients with other illnesses don't."
Patients were waiting for the procedure at home or in hospital even before the pandemic, Clifford pointed out.
"You have to mentally be prepared for delays,” he said. “Even if you get in hospital, this business of bumping can cause tension within a ward."
HUMAN RESOURCES MUCH HARDER TO FIND
Even if the province could find and buy a slew of new ECMO machines, there’s no way for it to play catch-up on open heart surgeries by running operating rooms for longer hours, the way the province has sought to clear other surgical backlogs.
Among the specialists required to run ECMO machines are perfusionists, who require years of training and were already in short supply when the acute care system wasn’t strained by hundreds of COVID-19 patients.
“It is not a problem that can be quickly fixed,” said David Bieber, spokesperson for the Health Sciences Association, a union representing skilled medical workers in B.C.
"This is a problem that predates the pandemic, because the fact is that we've had a couple decades now of a very austere approach to wage settlements for public sector workers in the health-care system and as a result, in many cases, they are earning less (in B.C.) than they could in other provinces.”
Like nurses and other frontline workers, Bieber says, perfusionists, respiratory therapists, technicians and others his union represents are burning out, with many considering leaving the health-care field after 15 grueling pandemic months.
“They're working very high levels of overtime and most have not taken a day or two off in terms of vacation for over a year; it's completely unsustainable,” said Bieber, though he did applaud the province for taking steps to start resolving the issue longer-term.
“They have dedicated money to provide new training seats for a lot of these professions and that's a step in the right direction,” he said. “We're hopeful that they will move quickly in terms of dealing with the lagging pay.”
With no easy solution in sight and the province declining to discuss how they see catching up on an open heart surgery waitlist that keeps growing, patients are left to wait anxiously to see where they fit in on the priority list.
“Critical heart is like critical COVID,” said Clifford. “I guess somebody's got to decide what goes where.”
CTVNews.ca Top Stories

'It could be catastrophic': Woman says natural supplement contained hidden painkiller drug
A Manitoba woman thought she found a miracle natural supplement, but said a hidden ingredient wreaked havoc on her health.
WATCH Video shows dramatic police takedown of carjacking suspects chased through parking lot north of Toronto
Police have released video footage of a dramatic takedown of a group of teens wanted in connection with an attempted carjacking in Markham earlier this month.
After hearing thousands of last words, this hospital chaplain has advice for the living
Hospital chaplain J.S. Park opens up about death, grief and hearing thousands of last words, and shares his advice for the living.
DEVELOPING G7 warns of new sanctions against Iran as world reacts to apparent Israeli drone attack
Group of Seven foreign ministers warned of new sanctions against Iran on Friday for its drone and missile attack on Israel, and urged both sides to avoid an escalation of the conflict.
WHO likely to issue wider alert on contaminated cough syrup
The World Health Organization is likely to issue a wider warning about contaminated Johnson and Johnson-made children's cough syrup found in Nigeria last week, it said in an email.
Tesla recalling nearly 4,000 Cybertrucks because accelerator pedal can get stuck
Tesla is recalling 3,878 of its 2024 Cybertrucks after it discovered that the accelerator pedal can become stuck, potentially causing the vehicle to accelerate unintentionally and increase the risk of a crash.
'It was all my savings': Ontario woman loses $15K to fake Walmart job scam
A woman who recently moved to Canada from India was searching for a job when she got caught in an online job scam and lost $15,000.
A couple lost their wedding rings during the ceremony. Two strangers found a fitting solution
Every good wedding has to have one teensy, tiny crisis.
Families to receive Canada Child Benefit payment on Friday
More money will land in the pockets of some Canadian families on Friday for the latest Canada Child Benefit installment.